Abstract

Introduction:
The estimated number of newborns with sickle cell disease (SCD) globally will increase from about 300,000 to more than 400,000 by 2050 according to current projections. Improved newborn screening, better supportive care, use of hydroxyurea therapy have decreased early childhood mortality among individuals affected with SCD, but the mortality in affected adults remains largely unchanged. Despite hematopoietic stem cell transplant (HCT) being curative in SCD, its impact on disease free survival remains unknown, partly due to limitation in donor options and perceived mortality in adults using myeloablative conditioning. Novel non-myeloablative and reduced intensity conditioned protocols have made HCT available to adult SCD patients who were previously excluded. Compared to the disease burden, HCT attempts globally is relatively small. Primary reason for this disparity is the non-availability of adequate donors, referral bias, procedure risks, costs and limited logistic resources in both the developed and the developing world. Our study focuses on recent outcomes of HCT for adult patients with SCD, with particular emphasis on comparative outcomes in pediatric patients transplanted for severe SCD.
Methods:
A comprehensive electronic search was conducted based on strict selection criteria for studies for meta-analysis. Adults, older than 16 years with SCD of all phenotypes, both genders and in all settings. All pediatric SCD studies were excluded. Outcome measures include:median overall survival (OS), freedom from treatment failure (FTF), mortality (overall and at 100-days, and 1-year post-HCT), transplant-related mortality (TRM), acute graft versus host disease (aGVHD), chronic graft versus host disease (cGVHD), progression free survival (PFS), incidence of late organ complications, graft rejection with recurrence or persistence of SCD. We found 391 articles with the above-mentioned keywords, out of which 177 were shortlisted and among these only 28 articles met our inclusion criteria.
Results:
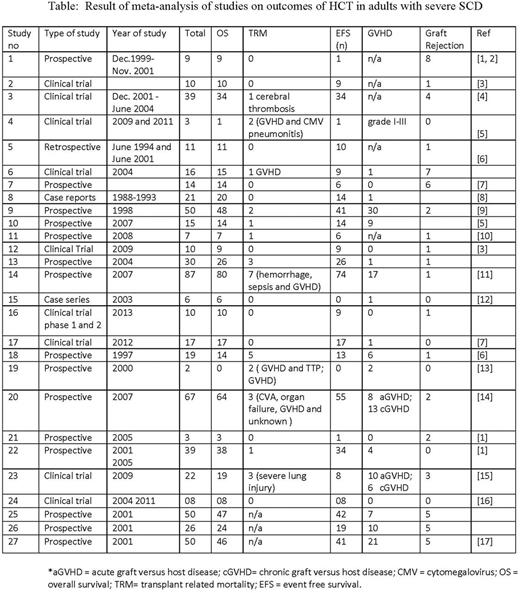
GVHD: In 28 studies, only 16 showed the presence of GVHD in adults, while only five studies showed a high incidence of severe GVHD as in Table 1.
Graft Rejection: We did not find a high incidence of graft rejection compared to historical controls in pediatric populations, however, multiple exposures to the blood transfusion prior to HCT and usage of chelation therapy for iron overload in the body system due to the repeated blood transfusion were found to be associated with increased incidence of graft rejection. Adult HCT studies showed a very low incidence of graft rejection once above-mentioned risk factors had been controlled (tables 1 and 2).
OS: We observed a similar transplant outcome, seen in pediatric HCT for SCD, were the unavailability of a healthy HLA-identical sibling lead to alternate donor transplantation, with associated increase in overall mortality, though no association was found on overall survival in relation to age of patient. Nine studies reported median OS of 100%, and two studies found a 70-80% overall survival (tables 1 and 2).
PFS: Sixteen studies included in our study revealed an acceptable PFS of more than 90%, whereas four studies revealed PFS of below 90% (87%, 85%, 82%, and 68% respectively) (table 1).
TRM: We observed that TRM has significantly reduced over the past few years. Most optimum outcomes were observed when recipients had good functional status at baseline. The main causes of death in transplanted patients were found to be sepsis, hemorrhage, severe lung injury and CNS hemorrhage with organ failure (table 1-2)
Conclusions:
Clinical data from current studies in our review demonstrate improved outcomes using HCT as a curative therapy for adults with SCD. However, lack of suitable HLA-identical sibling and matched unrelated donors severely limits accessibility of HCT therapy for eligible adults with SCD. Encouraging preliminary results using umbilical cord blood and haploidentical transplantation for SCD may solve the problem of this rarity.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal